Vitamin D Supplementation: Is It Safe or Even Necessary?
Vitamin D Supplementation Boom
Vitamin D supplementation has become far more commonplace in recent years, as awareness of it has grown to be almost as ubiquitous as Vitamin C. You may be taking it yourself, but have you been armed with all the available information to make sure your efforts are not wasted, or potentially harmful?
Let’s break down the entire background and physiological role of Vitamin D so that you can make an informed decision on whether or not supplementation is optimal, or even necessary.
This History Of Vitamin D
The role of Vitamin D in the body was accepted as vital amongst leaders in the conventional medicine space thanks to the history of rickets in the late 19th century, early 20th century. At that time, 80–90% of children in some industrial cities developed rickets in due to limited sun exposure and poor diet. When exposure to UV light proved to be the cure for rickets in 1919, scientists were able to link it to sunlight.
Not long after in 1922, lmer McCollum isolated the compound responsible and named it “vitamin D” after demonstrating that certain fats (like in cod liver oil) prevented rickets in animals. This prompted the widescale fortification of foods with Vitamin D in the 30’s to prevent this bone-deforming disease. Rickets vanished from society and Vitamin D lived happily in fortified cow’s milk and breakfast cereal.
Although vitamin D’s role in bone health was accepted mid-century, interest and research in its broader physiological roles such as its impact on the immune system and links to chronic disease spiked in the 1980s, and increased steadily into the 2010s, with a boom between 2005 and 2014.
Why this sudden interest, you ask?
Simply, infectious diseases were no longer in the spotlight as chronic and autoimmune diseases were on the rise (both thanks to vaccines and antibiotics? A topic for another day).
More attention turned to chronic, lifestyle-related diseases such as:
Cardiovascular disease
Cancer
Diabetes
Mood disorders
Vitamin D receptors were found throughout the body in the 1990s, including immune cells. This discovery positioned vitamin D as a single, inexpensive variable that might explain multiple chronic disease patterns making it extremely attractive to researchers. Vitamin D was easy to standardize, simple to dose, and wholly unpatented, yet highly marketable in supplement form–a pharmaceutical researcher’s dream.
Not only was research becoming popular and inexpensive, but so was testing Vitamin D levels.
Vitamin D blood testing became cheap, standardized, and widely available. Large population surveys began showing an alarmingly high percentage of people labeled “insufficient” or “deficient”, especially in northern latitudes with limited sunlight, elderly populations, and indoor workers.
This created a self-reinforcing cycle:
More testing → more low results → more concern → more research → more testing
Low vitamin D levels became framed as a public health issue, driving funding and publication volume. NIH funding for vitamin D research rose through the late 2000s, peaking at over $50 million in 2013 to accommodate the increased interest. The large budget produced a staggering body of research.
Another reason for increased interest in the “sunshine vitamin” was an unintended consequence of fear-mongering around skin cancer from sun exposure. Public health messaging in the 1980s–1990s heavily emphasized sunscreen use and/or total sun avoidance to reduce skin cancer risk. By the 2000s, researchers began questioning whether reduced sun exposure and increased use of sunblock was contributing to widespread vitamin D insufficiency.
Vitamin D essentially became a proxy marker for modern living, making it socially relevant beyond nutrition alone.
Routine blood tests in family medicine lead to widespread D2 (ergocalciferol) or D3 (cholecalciferol) prescriptions, often in 2,000-50,000 IU doses without any deeper understanding of its presence in body tissues or bio-personalization. (For perspective, we are expected to get around 600-800 IU or 15-20 mcg daily for maintenance needs. IU = International Unit, mcg = micrograms; 1 mcg = 40 IU. )
While D is indeed vital for healthy bones and immunity, blanket supplementation ignores important individual factors like metabolic types, tissue mineral balances, and risks like excess calcium deposition--a known effect of excess Vitamin D dosing, especially in the absence of Vitamin K2.
Is Vitamin D A Vitamin Or A Hormone?
Vitamin D Needs To Be "Activated" First
While we are going to continue calling it "Vitamin" D, this micronutrient actually behaves more like a steroid hormone in the body instead of a vitamin.
When you consume vitamin D from food or supplements or produce it in your skin from sunlight it is in an inactive form. In other words, your body must convert it through a multi-step process.
Vitamin D is first converted into 25-hydroxyvitamin D (the form measured in blood tests) in the liver. It is then converted into its active hormonal form, 1,25-dihydroxyvitamin D (calcitriol) as it moves through the kidneys. Wild, huh
This conversion process mirrors how hormones like thyroid hormone or cortisol are produced, activated, and regulated.
In contrast, typical vitamins are consumed, absorbed, and immediately utilized. Excess is excreted (with the exception of Vitamin A, which also has some hormone-like features).
Vitamin D Signals Cells Instead of “Feeding” Them
The active form of vitamin D doesn’t just participate in reactions. It binds to vitamin D receptors (VDRs) found in cells throughout the body, found in bone, muscle, brain, pancreas, reproductive organs and immune cells.
When vitamin D binds to these receptors, it turns genes on or off, influencing how cells behave–not typical vitamin behavior.
It Regulates Calcium Movement, Not Just Absorption
Vitamin D doesn’t merely help you absorb calcium from food, it helps direct where calcium goes: Into bones and teeth when mineral balance is healthy or into soft tissues when regulatory systems are stressed.
This is why vitamin D requires magnesium and vitamin K2 to function safely. Without these cofactors, vitamin D’s hormonal signaling can increase calcium movement and tissue deposits without proper control.
Hormone characteristics don’t stop there...
Vitamin D has system-wide effects specifically on endocrine activity. Some include interactions involve:
An impact on phosphorous levels, and ultimately, the relationship between calcium and phosphorous can have a sedative effect on the nervous system and metabolic rate.
Immune tolerance and inflammation
Insulin sensitivity modulation
Neurological signaling
Sex hormones like estrogen and thyroid function
Because vitamin D behaves like a hormone:
More is not always better
Its effects depend on receptor sensitivity and cofactors
High doses can create imbalance rather than correction
Supplementing vitamin D without assessing mineral status, liver and kidney function, or metabolic type is more akin to taking a hormone blindly than “just adding a vitamin.” High doses can likely create more of an imbalance rather than a simple correction by reducing a perceived deficiency.
For instance, HTMA results may indicate a calcium “shell” pattern that emerges when calcium levels in the hair register at greater than 75 mg (when 40ish is ideal). This excess of calcium signals poor cellular absorption of pretty much all materials in and out of the cell. Adding D to the mix can actually worsen this shell pattern, not correct a deficiency. If you were my client with high tissue calcium, I would highly advise against supplementing with D.
The effects of vitamin D really do depend on receptor sensitivity and the presence of cofactors (and whether those cofactors are able to be utilized!)
You see, things aren’t quite as simple as you’ve been told.
Understanding Vitamin D Blood Levels
Low Vitamin D Levels vs. True Deficiency: What Your Blood Test Really Means
To make matters more confusing, what you are told is a “Deficiency” in the blood may not necessarily be so. When people are told they’re “vitamin D deficient,” it’s almost always based on a single blood marker: 25-hydroxyvitamin D (25-OH-D). While this test is useful, it doesn’t tell the whole story and low numbers don’t always mean your body is truly deficient.
Circulating Levels Are Not the Same as Cellular Sufficiency
Standard blood tests measure how much vitamin D is circulating in your bloodstream, not how well it’s being used inside your cells. Think of it like checking how much money is in your checking account without knowing whether your bills are actually getting paid.
A low circulating level can occur for several reasons that have nothing to do with a lack of vitamin D, including:
Poor absorption or fat digestion (a HUGE problem that is oft-overlooked)
Liver or kidney stress affecting vitamin D conversion
Chronic inflammation or infection
Mineral imbalances that prevent vitamin D from being activated (especially Ca/Mg and Ca/P)
Increased physiological demand due to stress or illness (which, if the case, we would expect to upregulate after the stress or illness resolves if all other factors are taken into account)
In these cases, aggressively supplementing vitamin D may indeed raise the blood value, but will fail to correct the underlying problem.
Why “Low” Doesn’t Always Mean “Deficient”
Since Vitamin D functions more like a hormone signaling system than a simple nutrient and must be activated via the liver and kidneys, then work in partnership with minerals and nutrients (namely magnesium, calcium, phosphorus, and vitamin K2), the process leaves plenty of opportunity for dysfunction or misfires.
If the above constituents are present in optimal amounts or the systems aren’t functioning well, vitamin D can remain “stuck” in circulation or push calcium into tissues where it doesn’t belong. This is why some people continue to feel fatigued, achy, or unwell even after their vitamin D levels improve on paper.
In other words, a low number may reflect poor utilization, not true deficiency. You're taking enough in, its getting converted, and then getting lost in the shuffle. Therefore, a higher number on paper does not guarantee better function or safety
Understanding Reference Ranges (and Their Limits)
Most labs label vitamin D levels as:
Deficient: below ~20 ng/mL
Insufficient: ~20–30 ng/mL
Sufficient: ~30–50 ng/mL
Functional (i.e, optimal): ~50-100 ng/mL
(But even in this last range, blood levels may be showing high while utilization is still poor)
The first three ranges are based largely on population averages and bone-related outcomes, not individual metabolism, mineral status, or long-term tissue effects.
Two people with the same blood level can respond very differently to supplementation depending on genetics, stress levels, digestive health, mineral reserves/balance, hormonal balance
This is why some individuals feel worse when supplementing, even when their labs suggest they “should” benefit.
This supports cause to test calcitriol levels for the active form in the tissues, calcitriol or 1,25(OH)2 D2. The values for here are similar.
Sufficient: ~24.8-81.5 pg/mL
Functional: 35-55 pg/mL
How to Interpret Your Vitamin D Level More Accurately
Instead of asking “Is my vitamin D low?”, better questions are:
1. Is my body able to activate and use vitamin D properly?
This depends on liver function, kidney health, and adequate magnesium. Don’t know how you stand here? A CBC panel interpreted through a functional lens along with HTMA will provide the proper insight.
2. Are my minerals balanced?
Vitamin D increases calcium uptake. Without proper mineral regulation, this calcium can accumulate in soft tissues instead of strengthening bones. HTMA results will clarify this and also inform proper supplementation.
3. Do my symptoms align with deficiency or with imbalance?
Fatigue, muscle weakness, and immune issues can stem from many causes, not just vitamin D deficiency. Keep a journal, stay tuned into your body and its signals. What if you feel totally great? What reason would you have to fix something that isn’t broke?
4. Am I testing trends, not just one snapshot?
Repeating labs after dietary and mineral support often tells a clearer story than immediately increasing the dose.
Who Is More Likely to Need Vitamin D?
It’s tempting to see suboptimal blood values and immediately get on the supplementation bandwagon. Surely someone would benefit from such intervention?
For some people, especially those with very low blood levels, vitamin D supplementation can indeed be helpful. But raising a lab value should never be the only goal.
Let’s take a closer look at the conditions that likely call for D supplementation.
1) Someone with very low blood levels (<10–12 ng/mL) likely has a number of factors aligning to their detriment. They likely are exposed to limited sunlight plus have an absorption issue. Supplementing with D3 (not D2) makes sense, but so does addressing the deeper issues of absorption. The minerals are most definitely out of balance at the cellular level and that imbalance precedes the D deficiency. Ignoring that imbalance is ignoring the root cause.
2) Folks with certain autoimmune conditions may benefit from monitored Vitamin D supplementation because of its function as a hormone in the body such as those with MS, Rheumatoid Arthritis, Hashitmoto’s, or Type I diabetes. These folks most definite require medical monitoring with supplementation.
3) Liver and gallbladder dysfunction/absence or fat malabsorption issues may also alter Vitamin D needs and synthesis in the body, further supporting the need for blood monitoring and holistic appraisal of one’s health picture before simply hyperdosing with D.
4) Monitoring the elderly for D deficiencies and those with absorption issues, whether poorly managed or not, may require supplementation under the close supervision of a provider.
5) Finally, those on certain medications may have altered D needs that their medical provider should be cognizant of, but as we all know, this isn’t always the case. If you are on steroids or anti-convulsants, make sure your D levels are monitored and discuss supplementation with your provider.
In short, most people should not be blindly supplementing as the current culture would have us all believe, even though fully half of the world’s population may appear “Deficient” on paper.
Who Might Not Respond Well To Vitamin D Supplementation?
Not everyone benefits equally from ramping up vitamin D. About 75% of people show slow metabolic patterns on hair tissue mineral analysis, where excess D acts sedatively, potentially slowing thyroid and adrenal output further, leading to fatigue instead of vitality.
High calcium-to-phosphorus ratios often signal this; pushing dairy or D here might deposit fat peripherally rather than aid weight loss. Always check blood 25-OH-D levels first, as needs vary by sun exposure, genetics, and stress.
Before supplementing, shore up foundations: balanced diet, sleep, stress management, and digestion.
A More Informed Supplementation Approach
Common Pitfalls of Routine, Blanket Supplementation and Best Practices
As indicated above, Vitamin D and its hormone-like behavior interacts with many materials and systems in the body. Without the proper cofactors to assist it in its function, health issues may compound not resolve.
Further, knowing the tissue mineral status (particularly magnesium and calcium balance) you can discern if supplementing with vitamin D might help or hinder your health.
Vitamin D requires the presence of magnesium to be utilized, and most people are deficient in this important mineral. The right form of mag in the optimal dose is necessary to operate as that important cofactor.
HTMA will reveal how well magnesium is showing up in the body and if additional supplementation is necessary. But nine times out of 10, if you’re supplementing with D, you should be supplementing with a highly absorptive form of oral magnesium or regularly apply a magnesium chloride topical spray.
Calcium can often be in excess in tissues where it's only accumulating and not being utilized-- especially in highly stressed folks--making extra D in the system exacerbate, not alleviate, cellular absorption issues.
Excess calcium needs to be countered with additional magnesium, if excess is indeed the issue. Only testing can confirm this.
The moral of the story? Most people will need to couple D supplementation with added magnesium if they decide to proceed with supplementation at all.
Same goes for K2. Without this important vitamin (that can have several forms and only one that can operate as a cofactor--K2-M7), high doses of D supplementation can result in depleted potassium stores or even liver inflammation
One of the most pressing variables is supplementing with the optimal form of Vitamin D. The synthetic D2 is far less effective and is needed in much higher doses to be synthesized by the body. The prudent approach is to take the D3 form combined with K2 (as many supplements are currently formulated) and to take it in conservatively low doses, 1,000 to 2,000 IU daily.
Many sources encourage mega-doses of D in 50k IU amounts, and while this can quickly elevate levels of D, it will, as mentioned, deplete magnesium and create a bigger issue.
If after starting a Vitamin D supplementation regimen, unexpected fatigue or muscle issues manifest, it may be from such newly created mineral imbalances. Pause the D protocol, but maintain magnesium and B vitamins. Monitor for symptom resolution.
Blood vitamin D levels should be monitored and fully explored regularly. This means order both the 25(OH)D serum test that reflects the inactive D stores in the blood and the 1,25(OH)2 D2 active form that is reflective of utilization and kidney function.
B Vitamin Notes
Outside of mineral balance, starting B Vitamin supplementation is a more conservative approach to attempt before D supplementation. This is because forms of vitamin B are required for Vitamin D to function properly and it increases demand on all forms of vitamin B in the body (that whole hormone action…) it makes sense to make sure this water-soluble vitamin family is in abundance to start.
Take home: Get adequate vitamin B from diet and consider supplementation.
Symptom Appraisal and Tracking
Staying on top of symptoms is always key when we decide to add supplements into our health regimen. Overall metabolic and digestive health is vital for understanding what is necessary in the first place. Minerals are the first place to look, not vitamin D.
Likewise, staying on top of those symptom patterns and recognizing if there is a response to the support you’re administering is part of the “test, don’t guess” foundation of healing: Are the patterns changing? Are symptoms changing? And if so, for the better or worse?
Tracking symptoms and patterns alongside blood and HTMA provides full-picture insights.
This approach reduces the risk of over-supplementation and helps ensure vitamin D is actually working for your body, not against it.
Best Approach for Supplementing Vitamin D:
Step 1: Test blood D levels + HTMA for calcium/phosphorus ratios.
Step 2: Foundations first (per Protocol Guide priorities): Diet, digestion, magnesium, B vitamins before D.
Step 3: Safe dosing is conservative 1,000-2,000 IU D3 + K2 for confirmed lows below 15 mg/lU; retest in 8-12 weeks. Pair with sun exposure and liver supports.
Getting D the Old-Fashioned Way: Sun Exposure and Food
The 90’s fad of demonizing UV rays and hence, the encouragement of slathering on the sunblock (most of which are ironically loaded with carcinogens) probably didn’t do anyone any favors.
Many skin cancers occur where the sun never reaches. So the root cause of melanoma and such is more complex than just UV light = Cancer. But that’s what we were fed.
The knee jerk reaction created or at least contributed a whole new problem. Chronic D deficiency. Coupled with our depleted nutrients from the soils and lower-value foods, we now have to put in more work to get what we need.
Here’s what you need to know:
Sun exposure varies by latitude, season, skin tone, age
Closer to the equator provides enough sun exposure to generate what you need.
The longer days of summer in temperate climates equate to more sun exposure if you spend time outside.
Darker skin tones have a harder time synthesizing D.
The older you are the harder it may be to convert inactive to active D (this is a correlation, and not necessarily a function of age)
Supplementation isn’t automatically safer than sun, or vice versa.
If you are still deficient in spite of these factors aligning optimally, either you’re living in a hole, wearing too much sunscreen, or you have a conversion problem that has nothing to do with sun exposure.
Bear in mind that our modern lifestyles of working indoors all day limit effective synthesis of Vitamin D from the sun. Nutrient and mineral depletion of our soils, food, and bodies contribute to the problem of synthesizing the inactive form of D to the active, usable form.
The point here is, if you get plenty of sun exposure, supplementing is probably not going to help either. You have a deeper problem that warrants exploration.
Is It Worth Trying to Get Vitamin D from Food?
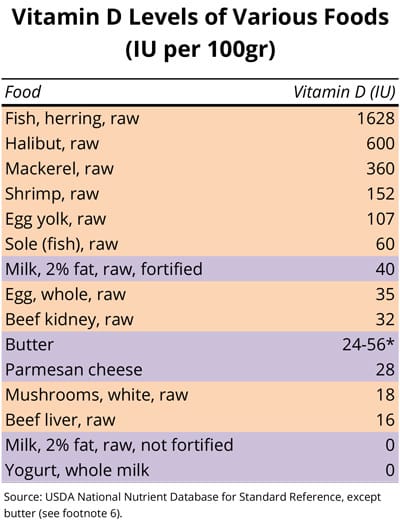
Food sources of Vitamin D do indeed exist, but are modest in both variety and dose.
Cod liver oil, which can be seen as a supplement in and of itself instead of a "food source", offers vitamin D alongside vitamin A (start with 1/4 tsp daily if tolerated), while fatty fish like sardines or salmon provide some D3 with healthy fats.
Egg yolks and liver add synergy too. These can support needs without overload, especially for fast metabolizers who burn energy quickly.
The amount you can obtain from food simply pales in comparison to what adequate sunlight would provide. However, when factors indicate that food-derivation should be prioritized, then by all means, prioritize.
Not quite.
Vitamin D aids calcium absorption, but excess--especially in slow metabolizers (75% of folks)--can promote calcifications or "calcium shells" seen in HTMA, weakening cellular function over time rather than building bone. Blood testing and mineral ratios matter more than "more is better."
Furthermore, without cofactors like Magnesium and Vitamin K2-M7, Vitamin D cannot be properly synthesized.
Not necessarily.
Low levels could signal magnesium deficiency (D activation needs it), genetic SNPs (mutations) in conversion, poor sun exposure, or even autoimmune needs. Blindly supplementing ignores patterns like high calcium or low potassium pushdown. Always test blood first and consider metabolic type.
Context matters.
High doses like 50k IU can backfire, especially with undetected calcium shells (e.g., calcium at 500 mg%), which conventional medicine simply doesn't test for. I've seen clients overloaded, with worsening fatigue or thyroid slowdown after megadoses of D.
Safe? Only if monitored with bloodwork and HTMA. Doctor scripts aren't typically tailored for your bioindividual needs like you think.



